Cancer care has become so complex that many physicians lack “core competencies in caring for patients with cancer,” warns a recent report, Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis, by the U.S. National Academy of Sciences Institute of Medicine (IOM). “Patients need to be asking, Is my doctor giving me appropriate treatment?” said cancer specialist Dr. Patricia Ganz of the University of California-Los Angeles. Gantz chaired the medical panel tasked with updating IOM’s 1999 report on the quality of U.S. cancer care. Progress has not been as great as hoped. “Barriers to achieving excellent care for all cancer patients remain daunting,” the new report notes.
Over the next two decades, an expected increase in new cancer diagnoses precipitated by the aging baby boomer generation and a predicted shortage of oncology specialists will make it more difficult to provide cancer patients with adequate care. But the growing complexity of cancer care in an age of genetic discovery is what most concerned the IOM panel.
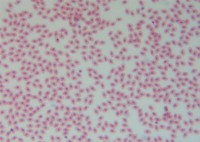
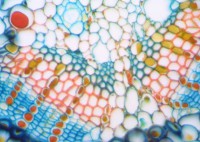
As scientists continue to explore the genetic mechanisms of cancer tumors and the importance of the tumor microenvironment, highly individualized cancer treatments are expected to become the norm. The IOM panel expressed concern that the volume and speed of new cancer discoveries appears to be outpacing the ability of many physicians to keep up with new knowledge and apply it to patient treatment. That knowledge/treatment gap is only going to widen as cancer treatment moves away from one-size-fits all chemotherapy and radiation treatments and toward modern advanced targeted cancer therapies tailored to meet the specific individual needs of each cancer patient.