Advances in cancer treatment allow for precision targeting of cells that cause damage. The flip side is that some cancers can become resistant to these traditional therapies. What are the factors behind this concerning development?
Mutations vs. Behavioral Changes
It’s well-established that cancer is a genetic disease. Changes in DNA, whether they’re random accidents or caused by carcinogens such as tobacco or UV rays, result in cancer by altering the way cells grow and multiply.
In some cases, cancer cells will mutate in such a way as to “dodge” the effects of treatment. However, in cases that doctors are observing with targeted chemotherapy, DNA remains the same and it’s the gene activity that changes. Epigenetic signals, a layer of regulators that control the activity of genes, are at the core of this new resistance.
Melamoma and Treatment Resistance
Scientists at the Systems Biology and Cancer Metabolism Lab at the University of California, Merced studied melanoma to gain some insight into this development. Melanoma is a particularly aggressive form of skin cancer that’s often caused by prolonged exposure to ultraviolet rays.
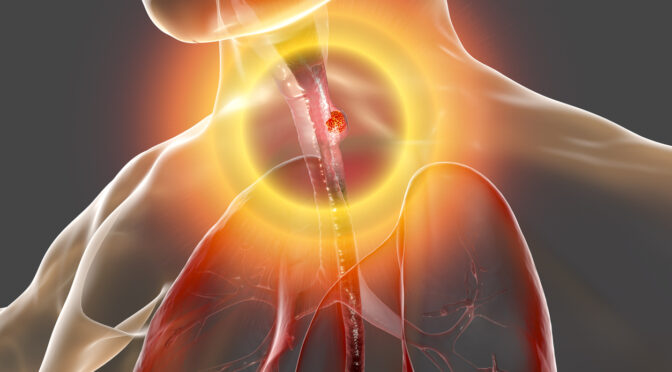
UV damage can cause mutations in a major signaling regulator known as BRAF. This protein is responsible for signaling cells regarding when to grow and divide and when to stop. Mutations triggered by UV rays cause BRAF to leave the growth signal turned on, leaving cancer cells to multiply unchecked.
Initially, targeted chemotherapy can successfully restore BRAF’s “off switch.” In some cases, rather than mutating further, cells “learn” how to bypass BRAF altogether, continuing their growth.
Personalized Cancer Treatment for Advanced Cases
At Issels®, our personalized immunotherapy programs have often achieved success after traditional methods have been exhausted. Visit our website for more information, including testimonials from patients in long-term remission after undergoing our non-toxic cancer treatment.