A common drug used in the treatment of arthritis may offer a new hope for cancer patients. At one thousandth of the cost of today’s latest blood cancer treatment, Issels® wanted to let you know about this important discovery.
The arthritis drug in question:
Methotrexate. A drug commonly used to treat inflammatory diseases such as rheumatoid arthritis, Crohn’s disease, and psoriasis. A World Health Organization ‘Essential Medicine’, the drug is well-understood, and if results are confirmed, could be used for treatment throughout the developing world. A one year course of low-dose treatment: $46. The cost for a single 60 tablet bottle of the current treatment, ruxolitinib: over $9,000. It is so costly that many retail pharmacies refuse to stock it.
What is it being purported to treat?
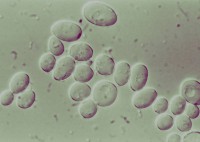
Myeloproliferative neoplasms (MPN). Typically seen in the 50-70 age range, MPN causes an overproduction of blood cells in the body. Symptoms include night sweats, itching, and tiredness. Though ruxolitinib has been developed for the treatment of MPN, it prices itself out of the market for most patients, whose treatment is otherwise limited to aspirin, excess blood removal, and chemotherapy.
What’s next?
Though further testing following the research performed by U.K.’s University of Sheffield confirmed the results, clinical trials are now being scheduled at Royal Hallamshire Hospital. Once complete, the new course of treatment with the repurposed drug could offer financial relief not only patients, but local and regional healthcare systems as well. The study could spawn research into the repurposing of other, previously safety tested, prescription drugs.
Are your cancer treatment options overwhelming your budget? At Issels® , you have options. Contact us today.