Gut bacteria, or microbiome, include organisms that manufacture vitamins and promote healthy digestion and other functions. A study recently published in Cancer Discovery found that pathogenic gut bacteria can have a negative impact on pancreatic cancer treatment.
When Gut Bacteria Fights the Immune System
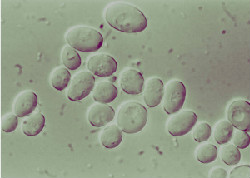
A research team at NYU School of Medicine conducted tests on both mice and humans with pancreatic ductal adenocarcinoma (PDA), a particularly aggressive form of pancreatic cancer. The scientists discovered that pathogenic, or “bad,” gut bacteria migrated to the pancreas, increasing bacterial presence by a thousand times.
Problems arise when this unbalanced mix of bacteria triggers a shutdown of immune cells, allowing cancer cells to multiply unchecked. Checkpoint inhibitors are a type of immunotherapy cancer treatment that reactivates immune cells, but they’re ineffective against the overwhelming amount of bacteria in the pancreas.
Using Antibiotics to Supplement Immunotherapy
When the researchers treated the mice with antibiotics, the amount of bacteria decreased enough to “flip the switch” on immune cells, thereby slowing cancer growth. In addition, checkpoint inhibitors were approximately three times more effective when used in conjunction with antibiotics.
Checkpoint inhibitors had previously failed to treat pancreatic cancer in clinical trials, so scientists are encouraged by these results. The team is now recruiting PDA patients to test the antibiotic-checkpoint inhibitor combo.
Issels®: Cancer Treatment Harnessing the Power of the Immune System
Our non-toxic immunotherapy programs focus on helping your body’s own immune system attack and kill cancer cells. These personally tailored treatments have fewer side effects and work to eliminate the causes that create tumors. Contact us for more information.





