Prostate cancer is the second most common cancer in U.S. men, with 1 in 7 being diagnosed. Experts now say that there are five distinct types of prostate cancer. How can this help you in your prostate cancer battle? Issels® Center for Immuno-Oncology wants you to know…
Identifying the pieces
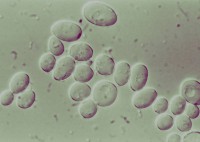
In the landmark study, samples of healthy and cancerous prostate tissue from over 250 men were analyzed, looking for abnormal chromosomes and measuring the activity of 100 different genes linked to the disease. Tumors of five distinct types were uncovered, each with a unique genetic fingerprint.
Putting the puzzle together
Prior research had identified six of the genes associated with prostate cancer, however the other 94 remained in hiding until brought to light by this recent study.
Solving the puzzle
The findings from this study could dramatically change the way prostate cancer is treated in the future. In identifying characteristics of the tumors, the scientists in the study were able to be more accurate at predicting aggressive, rapidly spreading cancers than today’s tests, such as the PSA test and Gleason score.
The missing piece
Current treatment methods, which result in some patients getting unnecessary treatment (and having to manage side effects) while others with more aggressive forms of prostate cancer often go without the intensive treatments they need will be impacted by this important study. The study findings could save lives by allowing doctors the opportunity to quickly identify specific cancer subtypes. This specialized classification may allow a more fitting course of treatment for each patient and help those identified with the aggressive classification of prostate cancer to get treatment faster and earlier. Before this typing of prostate cancer tumors can be used to start saving lives however, a larger trial needs to be done.
Looking for a center for immune-oncology that can handle every healthcare variable? Issels® has you covered! Contact us today.