Doctors have found some success with immunotherapy for cancer during the late stages of the disease, but the mystery of what causes certain tumors to spread has remained unsolved. Scientists are now turning to a surprising source for information about breast cancer progression.
A Matter of Engineering?
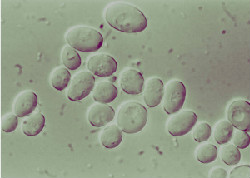
Ovijit Chaudhuri, an assistant professor of mechanical engineering, has been working with researchers across campus exploring the mechanical properties of breast tissue and their role in cancer progression. According to Chaudhuri, evidence supporting this relationship has been accumulating over the last 20 years.
Questions being studied by the teams include:
– How does stiffness of breast tissue encourage the growth and spread of tumors? Chaudhuri’s group is culturing mammary cells inside a hydrogel and tuning its stiffness to determine how it affects the development of cancer cells.
– How do cancer cells find their way past the membrane surrounding breast tissue that is seemingly too dense to allow passage? Currently, the scientists theorize that the cells use a combination of enzymes and force to “cut” their way through.
– As surrounding tissue grows in stiffness over time, how do tumors find space to expand?
Mechanobiology: A Complementary Approach
This isn’t the first time that scientists have sought biological information from the field of engineering. The result is the hybrid science of mechanobiology, which studies the interactions of mechanical properties and biological processes.
Immunotherapy for Cancer: Treating Resistant Tumors
At Issels®, our non-toxic immunotherapy programs have helped patients with advanced and therapy-resistant cancers achieve long-term remission. Visit our website for more information about our successful history of personally tailored and integrative cancer treatment programs.