When it comes to your health, viruses are usually thought of as something to avoid. New studies have shown that infecting tumors with viruses can actually boost the beneficial effects of immunotherapy for cancer.
Helping the Immune System Target Tumors
Your body’s immune system is the primary line of defense against invading cells. One of the barriers to successful cancer treatment has been the ability of cancer cells to evade detection, leaving them free to grow unchecked.
On the other hand, the immune system has an excellent ability to recognize viruses. Two separate studies show evidence that cancer-targeting viruses might be able to trigger an immune attack on tumors.
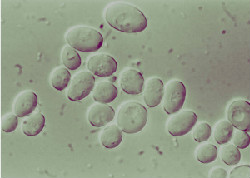
– A team in England injected nine brain tumor patients with a cancer-seeking virus. After the tumors were surgically removed, researchers discovered that the viruses had indeed reached their target, and there were signs that the viral infection caused an immune response.
– Researchers in Canada performed similar tests on mice with breast cancer. The virus was injected directly into the tumors, and while it had little effect on survival rates, the infected mice had fewer instances of tumors spreading.
Viruses and Immunotherapy for Cancer
Professor John Bell, senior author of the latter study, explained that the virus “raises a big red flag” to alert the immune system. He went on to say that the addition of a checkpoint inhibitor enables a full-force immune attack.
State-of-the-Art Immunotherapy Treatments at Issels®
The non-toxic, individually developed immunotherapy for cancer treatments at Issels® are directed at enhancing the power of your own immune system. Contact us to learn more about our integrative programs.