Scientists are excited about immunotherapy for cancer because it supplements a patient’s own natural defenses of the immune system. Thanks to a recent study, researchers have made a discovery that could lead to more effective immunotherapy treatments.
What Is Adoptive Cell Transfer?
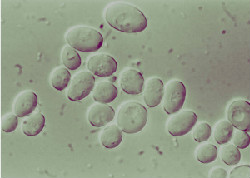
Adoptive cell transfer, one of the primary forms of immunotherapy for cancer, involves extracting a patient’s T-cells, which are a form of white blood cells that attack foreign invaders in the system. After engineering the T-cells to target the specific proteins in cancer cells, they are injected back into the patient.
While adoptive cell transfer has been successful in treating blood and bone marrow cancers, it’s been less effective with solid tumors. A team from The Scripps Research Institute and the University of California, San Diego set out to find a better way to program the T-cells.
Unleashing the Power of T-Cells
The researchers zeroed in on a protein known as Runx3, which appeared to specifically direct T-cells to solid tumors. During testing on animal models, it was found that overexpression of Runx3 led to delayed tumor growth and longer life.
Matthew Pipkin of Scripps said that Runx3 works on chromosomes within T-cells, enabling them to focus on killing tumor cells. Pipkin was hopeful that their discovery would pave the way for improving the effectiveness of adoptive cell transfer on solid tumors.
Issels®: The Leader in Immunotherapy for Cancer
Our proprietary immunobiologic core protocols are specifically designed to meet each patient’s individual needs. Contact us to learn more about our record of helping patients achieve and sustain long-term remission.





